Clinical Care Transformation
Consulting Services for Clinics: A Transformative Approach by Converging Health
Converging Health’s consulting services empower clinics to revolutionize their care delivery by moving to an advanced primary care delivery model. Designed for health systems, IPA’s or ACO’s entering into risk or value based payment models like Making Care Primary (MCP) or ACO Flex, the services focus on transitioning from reactive fee-for-service models to proactive, value-based care systems. The goal is clear: improve patient outcomes, reduce costs, and boost clinic profitability while enhancing the joy of practicing medicine.
Converging Health helps primary care practices boost profitability while improving patient care by helping to decrease unexpected high costs from missed opportunities, greatly eating away potential cost savings. Their services focus on risk management using robust analytics, identifying high-risk patients for targeted care, and implementing optimized care pathways to enhance outcomes and reduce costs. They transform teamwork by redefining roles, enabling clinicians to build patient trust, and support financial optimization through accurate risk coding and cost-saving strategies. With training, consulting, and proven results—such as reduced hospitalizations and ED visits—Converging Health empowers clinics to achieve sustainable care transformation and significant ROI.
Imperative for ACOs and health systems in value based payment arrangements, our clinical experts take this strategy to the next level with implementation, training, and metrics for performance assessment.

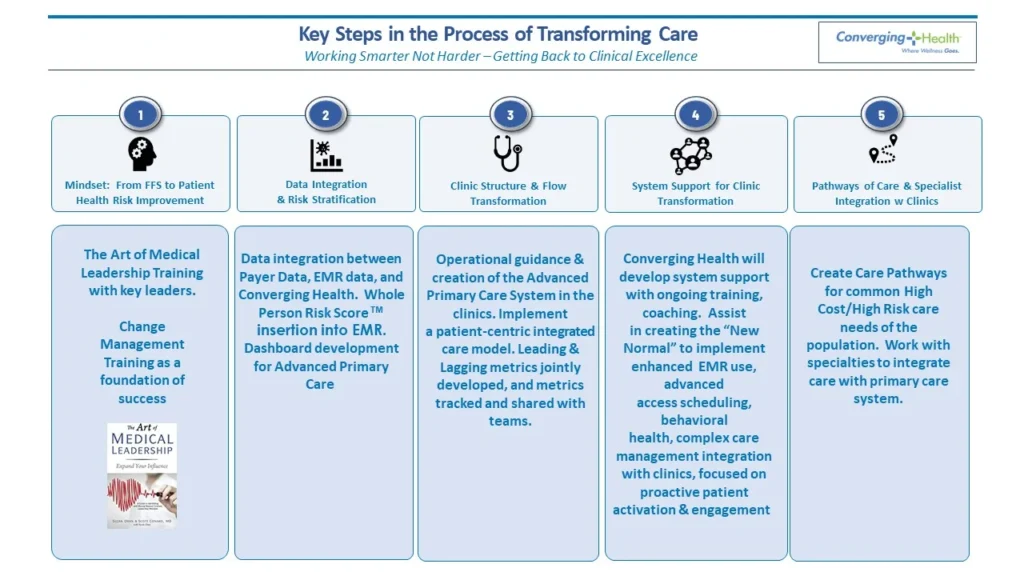
The Five pillars of transformation
The foundation of Converging Health’s consulting approach lies in its “Five Pillars,” a robust framework that supports clinics in systematically reshaping their operations
Mindset Shift
Clinics must transition from a fee-for-service mentality to a proactive, value-driven approach. This shift involves embracing preventive care, early intervention, and team-based management. Converging Health coaches clinic leaders to foster this transformation, ensuring alignment across teams and clarity in purpose.
Data Management
Data is the backbone of effective healthcare delivery. Converging Health integrates multiple data sources into a centralized system, enabling clinics to identify high-risk patients, track care gaps, and make data-informed decisions. Advanced analytics tools process electronic medical records (EMRs) and claims data to generate actionable insights.
Process Optimization
By redefining roles and workflows, Converging Health helps clinics streamline their operations. Clinicians can focus on trust-building and patient engagement while administrative tasks and care coordination are managed by support staff. This approach alleviates clinician burnout and enhances the efficiency of care delivery.
System Support
Clinics receive assistance in integrating key support systems, such as pharmacy services, mental health care, and social work. These wraparound services address the diverse needs of patients, enabling a holistic approach to care that reduces unnecessary costs and improves outcomes.
Vertical Integration
To retain patients within the clinic’s network, Converging Health establishes clear care pathways with specialists, imaging facilities, and other healthcare providers. This reduces patient leakage and ensures continuity of care, which is critical in a value-based care model.
Transformative Tools and Insights

Key to your success with Converging Health is the use of their Vison Hawk’s Whole Person Risk Score and MyPHA. Vision Hawk identifies the issues, and MyPHA solves them. The Whole Person Risk Score, combined with active outreach by MyPHA, ensures patients receive the right care at the right time, improving health outcomes while reducing overall costs.
Results in Action
Dramatic Cost Savings are Yours for the Taking
Converging Health’s model has delivered extraordinary financial results for its clients. A recent success story involved a safety-net hospital in New York City managing a high-risk Medicaid population. Through mindset shifts, data integration, and care pathway implementation, the client achieved:
- $18 million in savings over 15 months.
- An 11% decrease in inpatient days.
- An 18% reduction in emergency department (ED) utilization.
Program implemented in 2024
utilizing 40% of converging health's services
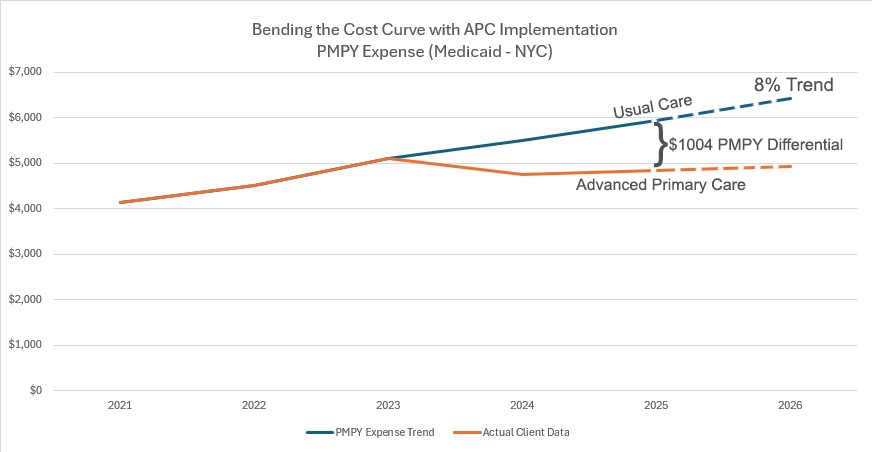
Overall, clinics working with Converging Health have seen cost reductions ranging from 9-10% in the first year to as high as 25-30% in subsequent years.
By addressing the root causes of high healthcare costs—such as unmanaged chronic conditions and delayed interventions—Converging Health helps clinics achieve lasting financial improvements.
Converging Health’s approach is distinct in its combination of consulting expertise and actionable tools. Clinics benefit from:
- Proven ROI: Clients report returns as high as 48:1 within three years of implementing Converging Health’s systems.
- Tailored Solutions: Each clinic receives a customized plan that aligns with its unique needs and goals.
- Sustainability: Converging Health trains clinics to “fish for themselves,” reducing reliance on consultants over time.
- Comprehensive Support: From mindset shifts to data analytics, Converging Health addresses every aspect of care transformation.
whole person risk score
The Whole Person Risk Score is designed to identify patients at high risk for adverse health events. By understanding the diverse factors contributing to risk, healthcare providers can implement targeted interventions to prevent future problems. This score also supports prioritizing patients for high-value visits—longer appointments focused on building trust and addressing complex health concerns. By integrating multiple data points, the Whole Person Risk Score provides a more holistic and predictive view of patient health, enabling a proactive and preventative approach to care.
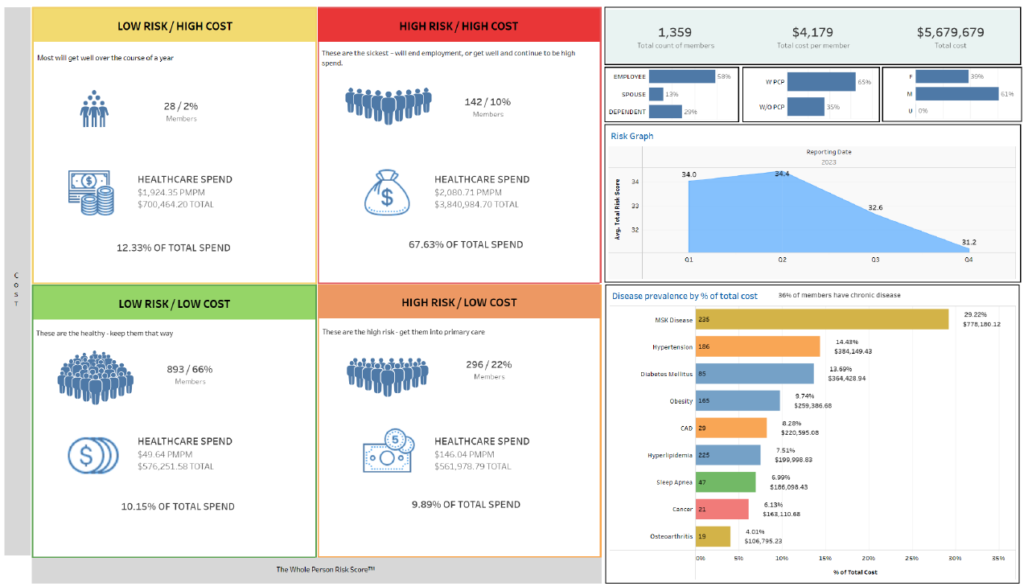
The risk score enables clinics to proactively engage patients through targeted outreach and “high-value visits,” which focus on comprehensive management of chronic conditions and preventive care. Clinics receive monthly lists of high-risk patients, empowering them to address needs before adverse events occur.
The Whole Person Risk Score is a comprehensive tool designed to assess a patient’s overall health risk by looking beyond medical diagnoses to include factors related to their engagement with their health. It consists of three key components:
Absolute Risk: This component evaluates a patient’s medical conditions, medications, number of healthcare providers, and social determinants of health. It offers a foundational understanding of the patient’s health status and potential risk factors.
Clinical Quality Risk: This component assesses the quality of care the patient receives based on established guidelines and care pathways. It identifies gaps in care and highlights areas where necessary treatments or preventive measures may be missing.
FLAIR (Functional Literacy and Activation in Relationship) Score: The most predictive element of the score, FLAIR evaluates a patient’s engagement with their health and the healthcare system. It takes into account factors such as health literacy, whether the patient is proactive or reactive in seeking care, medication adherence, and their relationship with primary care.
How is the Whole Person Risk Score used?
Data-Driven Identification of High-Risk Patients:
The score is generated by analyzing patient data and helps identify those at high risk for adverse health events. It enables proactive outreach, prioritization of high-value visits, and the delivery of preventive care.Monthly Updates and Proactive Outreach by MyPHA:
The Whole Person Risk Score is updated monthly to create a dynamic list of high-risk patients. This list is used by MyPHA (Personal Health Assistants) to actively reach out to patients, ensuring timely scheduling of appointments, addressing care gaps, and providing ongoing support.Integration with Electronic Medical Records (EMRs):
The score is embedded in the clinic’s EMR system, providing the entire care team with access to this data. This ensures alignment in care delivery and fosters a team-based approach.Enhanced Care Planning and Engagement:
The score informs personalized care plans, closes care gaps, improves chronic disease management, and fosters patient engagement and trust.Improved Team Communication and Efficiency:
By providing a centralized risk assessment, the score enables better coordination and efficiency within the care team, promoting a team-based approach to patient care.Shift from Reactive to Proactive Care:
A key goal of the Whole Person Risk Score is to shift care delivery from reactive to proactive, identifying and addressing health issues before they escalate into more severe or costly events.Cost Savings Through Advanced Primary Care:
Using the Whole Person Risk Score alongside an advanced primary care model reduces hospitalizations, emergency visits, and other expensive events, resulting in cost savings of 9-30%, depending on implementation level and patient risk.Data Sources Supporting Comprehensive Care:
Data for the score is derived from insurance companies, Medicare, Medicaid, and EMRs, enabling a holistic view of the patient’s health. MyPHA uses this information to guide care plans, proactively close care gaps, and ensure accurate documentation of patient conditions.Focus on Patient Relationships:
The system empowers care teams to focus on building relationships with patients, while data drives informed medical decision-making. High-value visits are prioritized to foster trust and create effective care plans.
The Whole Person Risk Score, combined with active outreach by MyPHA, ensures patients receive the right care at the right time, improving health outcomes while reducing overall costs.
Getting Started
Comprehensive Implementation Process
The consulting process begins with a thorough assessment. Over three to four days, Converging Health evaluates the clinic’s current operations, including data systems, workflows, and team dynamics. A detailed report outlines strengths, weaknesses, and actionable steps across the Five Pillars.
From there, clinics embark on a tailored transformation journey:
- Initial Training: Clinicians and staff receive coaching on advanced primary care models, risk stratification, and data utilization.
- Pilot Programs: Clinics can test changes within a single location before scaling them across the system.
- Full Implementation: Over a period of 6-24 months, Converging Health provides ongoing support as clinics adopt new workflows, integrate systems, and optimize care delivery.
Converging Health’s focus on training staff and embedding processes ensures long-term sustainability. By the end of the third year, clinics are fully equipped to independently manage their value-based care models.
Empowering Primary Care
A core mission of Converging Health is to elevate primary care. Though we may be a bit biased, as our Practice Transformation team contains multiple Board Certified Family Practice Physicians with over 50 years total experience. Through all the changes in the world of healthcare, value based care has been by far one of the best. By shifting the focus from reactive, volume-driven care to patient-centered, proactive care, clinics can enhance their revenue while reducing clinician burnout. This approach positions primary care providers as leaders in the healthcare ecosystem, fostering respect, trust, and long-term success.
A Bold Vision for the Future
Converging Health’s consulting services are reshaping the healthcare landscape. By addressing the inefficiencies and inequities of the traditional models, they empower clinics to deliver exceptional care while achieving financial success. This isn’t just a transformation—it’s a revolution in healthcare delivery, one clinic at a time.
80% of ACOs are losing money
Financial Risks of Value-Based Care:
- Risk Management: Success depends on accurately assessing patient risk to ensure sufficient PMPM payments.
- Data-Driven Approach: Effective use of risk coding (e.g., Hierarchical Condition Category codes) is essential.
- Care Transformation Required: Old FFS workflows cannot simply be adapted—clinics must prioritize proactive, team-based care.
- Potential Financial Loss: Organizations assuming downside risk must implement advanced primary care models to mitigate financial and clinical risks.
- Systems & Infrastructure: Clinics must invest in identifying high-risk patients, proactive care strategies, and integrated care teams.
Keys to Financial Success in Advanced Primary Care:
- Cost Savings: Clinics implementing advanced primary care can achieve 9-10% savings in the first year, increasing to 25-30% over time.
- High ROI: Successful models report ROI after working with Converging Health as high as 48:1, demonstrating strong financial potential.
- Team-Based Care: Collaborative care models improve efficiency, reduce clinician burnout, and enhance patient outcomes.
- High-Value Visits: Longer, more targeted visits help close care gaps and prevent costly health issues.
Value-based care offers financial stability and rewards proactive, preventative care, but success requires strategic risk management, robust data systems, team-based workflows, and a shift from volume-based to outcome-focused care delivery.

