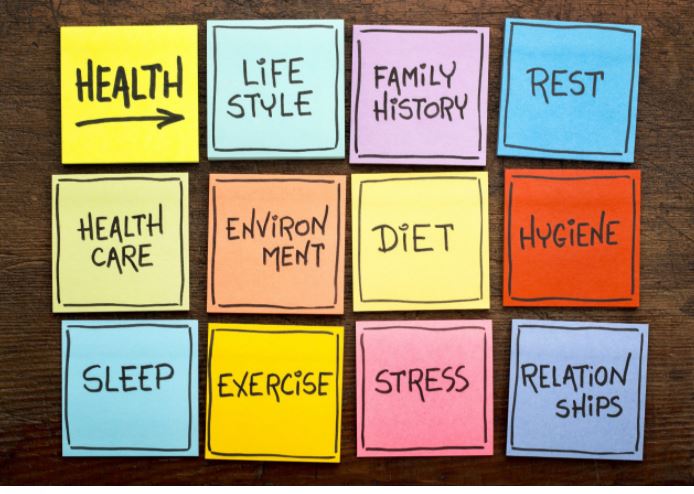
Moving from Fee for Service to Prospective Payment in Primary Care: Advanced Primary Care: The Future of Primary Care – Part 6 Sponsored by WWW.THEMDCEO.COM We believe that the clinicians’ philosophy of care and their scope of practice are foundational elements that create the opportunity for success in a prospective payment-based system. A whole person approach to healthcare is the approach that will produce the highest levels of health and well-being among the patients served. In a prospective payment model, the whole person approach will also produce the greatest financial rewards. The core idea of whole person health care, what’s most important in taking care of our patients, is to understand what matters most to them in their lives and making that the centerpiece of how we try to help with their lives and their health care. This differs from the FFS orientation which focuses on identifying and treating disease. For the clinician, we begin with our belief that each person has an “inner healer” that can be activated and supported as a patient responds to the forces that set him/her back. What kinds of skills and assistance does a patient need to help them move toward health and well-being? Using the power invested in the healer provides us a lever that can help the patient move forward. It is the patient’s beliefs and actions that matter most. We are their guides and a resource they can use. The “Jedi Warrior” believes in and can tap into the “force” for health and well-being and works to support the patient on their path towards health. This approach to care juxtaposes to the clinician as “car mechanic” who fixes body parts. We draw heavily on the work of several primary care thought leaders. Listed alphabetically Steve Bierman, MD is the author of “Healing Beyond Pills and Potions.” Dr. Bierman understands the tremendous impact of ideas on health and healing—ideas held by patients, and ideas delivered by caregivers. His approach has resulted in lasting cures of so-called chronic diseases, regression and disappearance of advanced tumors, bloodless and painless surgeries, and resolution of a wide array of “gray zone” syndromes that defy diagnosis. Scott Conard, MD is the author of “The Seven Healers” and other books The Seven Healers are seven specific ingredients that every human being needs in order to survive and thrive in this life. These essentials are not limited by a person s nationality, skin color, or religion. They are universally required by all. The Seven Healers, in order of their necessity for survival, are Air, Water, Sleep, Food, Play, Relationships, and Purpose. Without these time-tested elements, you cannot flourish and live a meaningful life. Once you identify the problem, you can trace it back to the root cause and find the answer. https://www.goodreads.com/en/book/show/16070555-the-seven-healers Wayne Jonas, MD is the author of “How Healing Works” Dr. Jonas is a champion of whole person and integrated care. He believes that healing is as important as curing. For Dr. Jonas, whole-person care addresses the four dimensions of a human being–physical, behavioral, social and emotional, mental and spiritual, and it is delivered in a person-centered way. He created the HOPE Note a tool to elicit the information needed from a patient to better understand their issues beyond the regular medical visit. The HOPE note builds off the SOAP (subjective, objective, assessment, and plan) note that every medical student learns and is applied every day in practice. The HOPE note is a patient-guided process designed to identify the patient’s values and goals in their life and for healing. The role of the physician is to provide the evidence and support to help them meet those goals. https://drwaynejonas.com/ James Mold, MD is the author of “Goal Oriented Medical Care” The premise of Goal-Oriented Medical Care is that, prior to consideration of strategies, the health care team must understand the patient’s personal health goals and priorities. The addition of the goal-clarification step changes the focus from problem-solving to goal attainment, forcing a reconsideration of the meaning of health and the purpose of health care. It elevates the role of patients in decision-making, broadens the range of strategies, encourages individualization and prioritization, and creates a conceptual framework for true person-centered care. And while the idea is deceptively simple, it provides a blueprint for the transformation of health care systems trying to adapt to changing health concerns, scientific and technological advances, health and health care inequities, and rising costs. Scott Morris. MD, MDiv. is the author of “Health Care You Can Live With: Discover Wholeness in Body and Spirit” Dr. Morris is the creator and leader of Church Health in Memphis, TN. He knows that hope, health, and healing happen when we consider the whole person. His model of care connects the dots across faith, medicine, movement, work, emotions, nutrition, and friends and family. Whether caring for patients or reaching out to the community, he holds high the dignity and worth of each person. The Church Health Model for Healthy Living recognizes that our lives are complicated. We are better together when we help one another access the quality health care necessary to live with dignity, vitality and joy. He believes that all health care delivery begins with love of patients. He has developed a Model for Healthy Living that is a tool for individuals to use to take charge of their own health, and it reflects that true wellness is not just about our bodies but about the interconnectedness of body, mind, and spirit in all the ways that we live. https://tinyurl.com/2cf62zxx and https://tinyurl.com/4c8u94pb Scope of Practice refers to the range of services that can be offered through the primary care practice. Can patients receive services such as simple dermatologic procedural services, sports medicine services, treatment of common musculoskeletal problems, (Osteopathic manipulation therapy, physical therapy, massage, Acupuncture, etc.) brief office counseling for mental/behavioral health issues, etc. The goal is “one-stop shopping” as much as possible. The final issue here involves helping the clinicians to reconnect with and renew their understanding of and commitment to their core values. It’s more than continuing