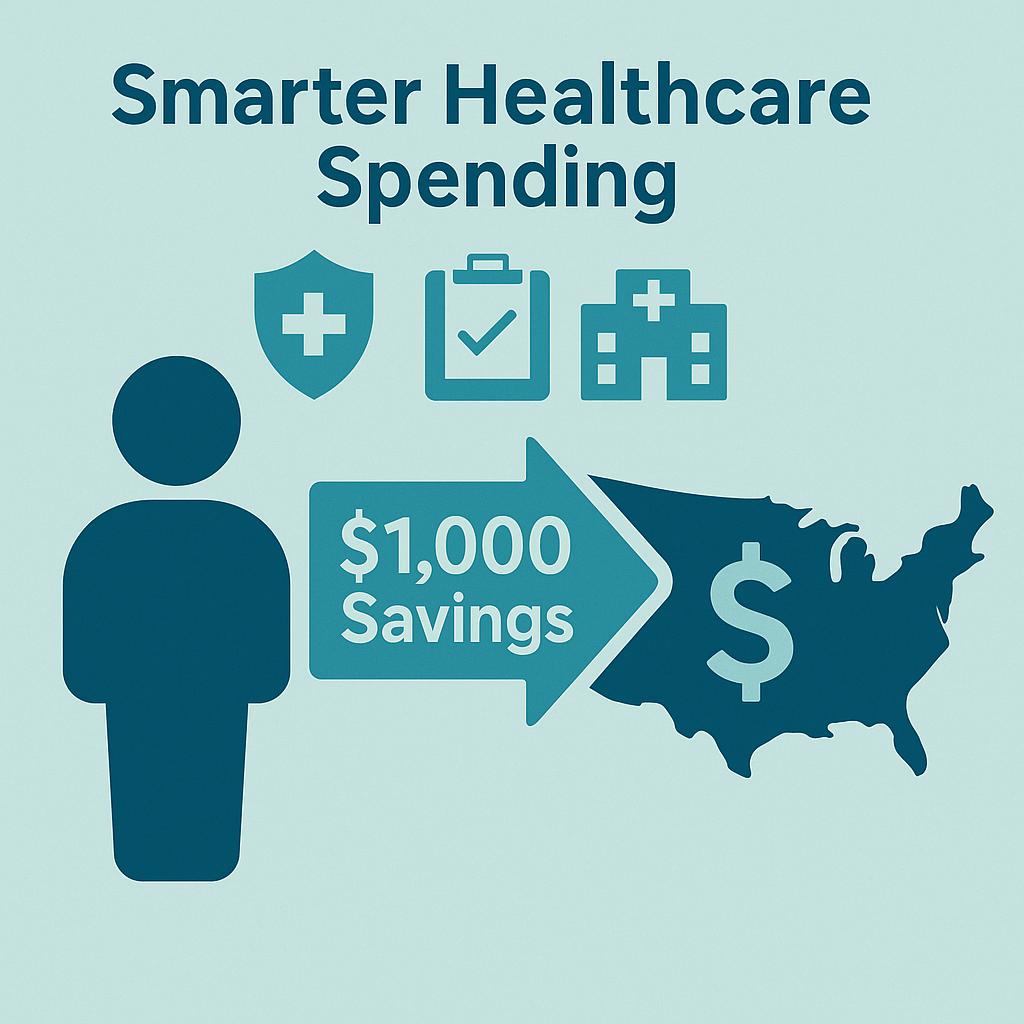
How our client spends $1000 less than U.S. Average PMPY
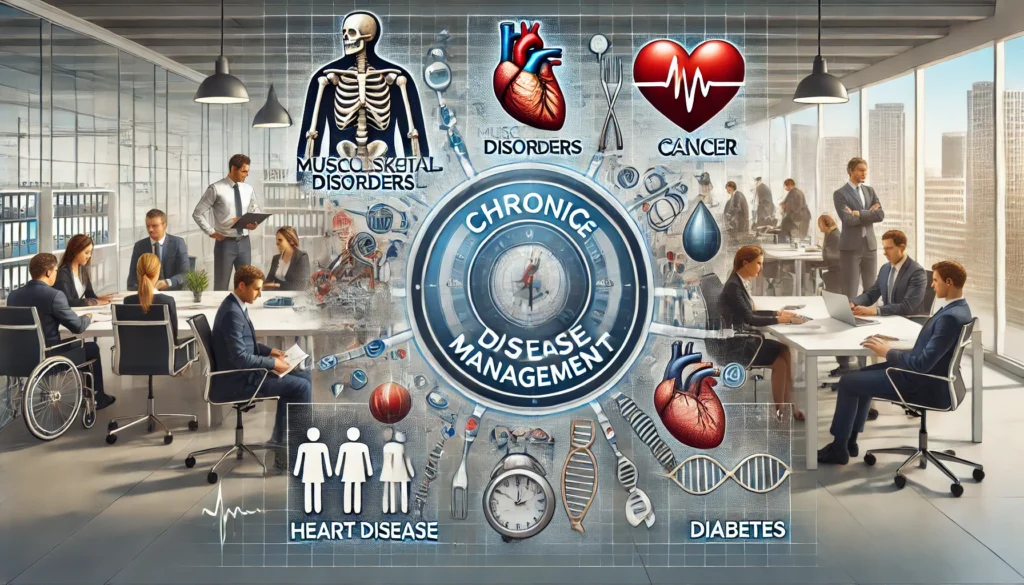
Rethinking ER Utilization: How Clinical Consulting Can Boost Profitability and Patient Outcomes Emergency room (ER) visits are climbing at an unsustainable pace—outstripping population growth and burdening healthcare systems across the country. For providers and clinics navigating shrinking margins, this trend isn’t just a symptom of patient behavior—it’s a call to action. As noted on the Relentless Health Value podcast, Al Lewis points out that “commercially insured individuals are visiting the ER at rates now exceeding 200 visits per thousand lives.” That’s roughly one ER trip for every person under 65 every four to five years—and that’s not including the elderly or Medicaid populations, where rates are often even higher. What’s driving this surge? A key culprit is limited access to timely, coordinated primary care. Dr. John Lee, an ER physician featured on Relentless Health Value, described the downstream effect vividly:“Patients arrive with symptoms they’ve had for months, unable to get in to see their PCP. We run CTs, labs, ultrasounds—all in one visit. We skip the prior auth headaches, but we also cram weeks of diagnostics into an afternoon. Multiply that by thousands—it’s no wonder ER volume has exploded.” This pattern of delayed care, over-reliance on emergency departments, and unnecessary diagnostics doesn’t just harm patients—it hits your clinic’s profitability and efficiency, too. A Smarter Way Forward: Clinical Consulting with Converging Health At Converging Health, we partner with healthcare organizations to break this cycle. Our clinical consulting services help practices and systems shift from reactive, fragmented care to proactive, coordinated strategies that reduce unnecessary utilization and drive down the total cost of care (TCOC). One of our community hospital clients is a case in point. Over the past five years, their cost containment trajectory has significantly outpaced national averages: Year Converging Health Client Expected Spend (based on US average Increase) March 2023 $5,102 PMPY 2023 Baseline March 2024 $4,749 PMPY $5,520 PMPY* March 2025 $4,986 PMPY $6,033 PMPY * *WTW’s Global Medical Trends Survey, the cost of medical care benefits in the U.S. increased about 9.3 percent in 2024, compared with 8.2 percent in 2023. Converging Health started working with this group in March of 2023. While national healthcare costs and Total Cost of Care (TCOC) are expected to jump by nearly $1,000 PMPY between 2023 and 2025, our client is projected to remain more than $1,000 below what they otherwise would be spending based on average U.S. increases in TCOC—a compelling return on investment. This isn’t just about suppressing numbers on a spreadsheet. It’s about reengineering care delivery to prevent unnecessary ER visits, improve patient engagement, and enable earlier intervention. This client achieved an 18.4% reduction in ER utilization and 21% reduction in Inpatient Days by implementing: This systematic, data-driven approach allows PHAs to steer individuals toward the most appropriate, cost-effective care—reducing risk, avoiding high-cost interventions, and improving quality of life. Or, as Relentless Health Value puts it:“Fix the front end of care, and you’ll save money on the back end. It’s that simple—and that hard.” The Bottom Line for Providers When your clinic loses patients to the ER, it doesn’t just lose revenue—it loses a chance to deliver higher-value care. Converging Health’s clinical consulting equips your team with the tools to reduce costs, improve outcomes, and protect profitability. Because healthcare doesn’t need to cost more to deliver more value. It just needs to be smarter. 👉 Learn more about how Converging Health’s Clinical Care Transformation services can support your practice at ConvergingHealth.com.
How our client spends $1000 less than U.S. Average PMPY Read More »